Darwin Demeny has always “The reason behind the screening lived an active lifestyle. He spent 30 years as a baseball, softball and soccer coach, and at 72 years-old he still enjoys completing home improvement projects of all sizes. But last fall his life changed when his first colonoscopy, prompted by unusual bowel movements, led to a Stage 4 Colon Cancer diagnosis.
“I had no signs of anything until I went in to get the screening,” Demeny says. “I probably should have gone in previously and had some screening done, but I’ve been healthy, I’ve been active, and I do a lot of physical stuff.”
This year brings a change to preventive screenings for colon cancer, the fourth most common cancer among men and women in the U.S.
The Centers for Medicare & Medicaid Services (CMS) recommended age for starting regular colon screening is now age 45, instead of age 50. And, if a non-invasive test shows a positive result, Medicare will now cover a follow-up colonoscopy, meaning no out-of-pocket costs for either test.
The move follows changes to screening guidelines from the U.S. Preventive Services Task Force aimed at finding and treating the cancer earlier, in the hope of saving more lives. About one in 23 men and one in 25 women will be diagnosed with colon cancer in their lifetime, according to the American Cancer Society (ACS). But caught early, it is highly treatable and often curable.
“The reason behind the screening is to catch polyps early where they can be removed, before they turn into an invasive cancer that needs more extensive therapy or surgery,” said Dr. Robert Delaune, an oncologist and hematologist with Minnesota Oncology, where he serves as medical director for the East Metro. “A lot of patients can be screened, have polyps removed, and reduce their risk of cancer.”
Though colon cancer is being seen at younger ages, it can also show up later in life, making screenings important all the way through age 75 and sometime beyond, depending on your risk factors. Delaune outlines those risks, colon cancer symptoms and screening options.
Know your risk
Some of the primary risk factors for colon cancer include:
• Family history — if you have an immediate family member — a parent or sibling — who had colon cancer.
• Other ailments — if you have
any kind of inflammatory bowel disease, such as Crohn’s disease.
• Poor diet — eating a diet high in red meat and low in vegetables.
• Lack of exercise — little or no regular physical activity.
• Alcohol use — having more than three alcoholic beverages a week.
• Smoking — particularly people who have smoked for a long time, are more likely to develop colon cancer.
Common symptoms
“The symptoms you’d be looking for are mainly a change in bowel habits,” Delaune says.
For example, signs might include a significant increase in constipation. Or, if you are experiencing lingering abdominal pain, or any type of rectal bleeding. Patients will sometimes mistake bleeding from colon cancer for hemorrhoidal bleeding. What’s most important is to look for anything that is out of the ordinary, and if you are unsure, it’s best to talk to your doctor.
It’s common for people with early-stage colon cancer to have no symptoms, which is why screening is important.
Getting screened
Though colon cancer is still a leading cause of death in the U.S., those rates have been dropping for years, largely because of the success of screenings. There are several ways to be screened for colon cancer. It’s best to talk with your doctor about your risks and what test is best for you.
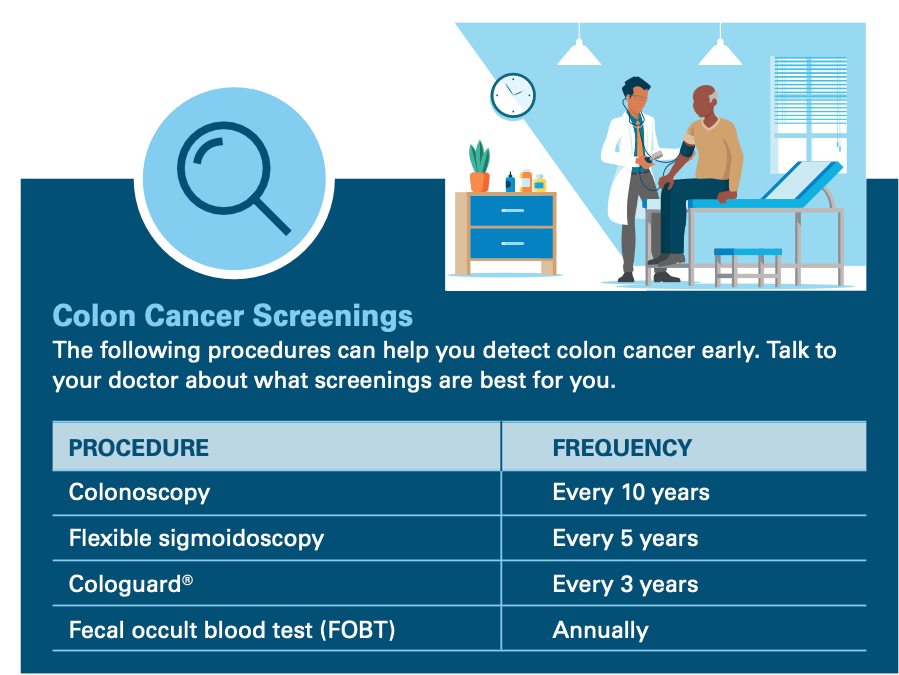
The ACS breaks screenings into two categories: non-invasive stool- based tests and visual exams that use a scope or X-ray. Examples of stool-based tests include Cologuard® and the fecal occult blood test (FOBT), which can be done in the privacy of your home. The most common form of a visual test is the colonoscopy, an in-clinic procedure that uses a scope to look for polyps. Another example is the flexible sigmoidoscopy, which is similar to a colonoscopy, but does not examine the entire colon.
There are pros and cons to each test and frequency recommendations differ for each. Though the invasive nature of colonoscopies make some people uneasy, Delaune says the process has become easier, particularly the preparation and recovery.
“What’s most important is that you get screened,” he says.
Treatment
Cancerous polyps can often be removed during a colonoscopy.
In other cases, surgery might be required, as well as a combination of chemotherapy, radiation therapy, or drug treatments. Delaune says treatments are advancing all the time, with some immunotherapy drugs showing the possibility of eliminating cancer without surgery.
“These are exciting times for treatment,” he says. “There are many options available.”
After three rounds of treatment, Demeny’s vitals and blood work are promising.
“If I was doing it over,” Demeny says, “I would’ve gotten checked earlier when I didn’t have any signs.”


