For more than three decades, horses were Karen Little’s passion.
“I actually spent most of my younger years riding horses,” says the Roseville resident, now 69. “And falling off of horses is one of the reasons why I have pain. That and a couple car accidents along the way.”
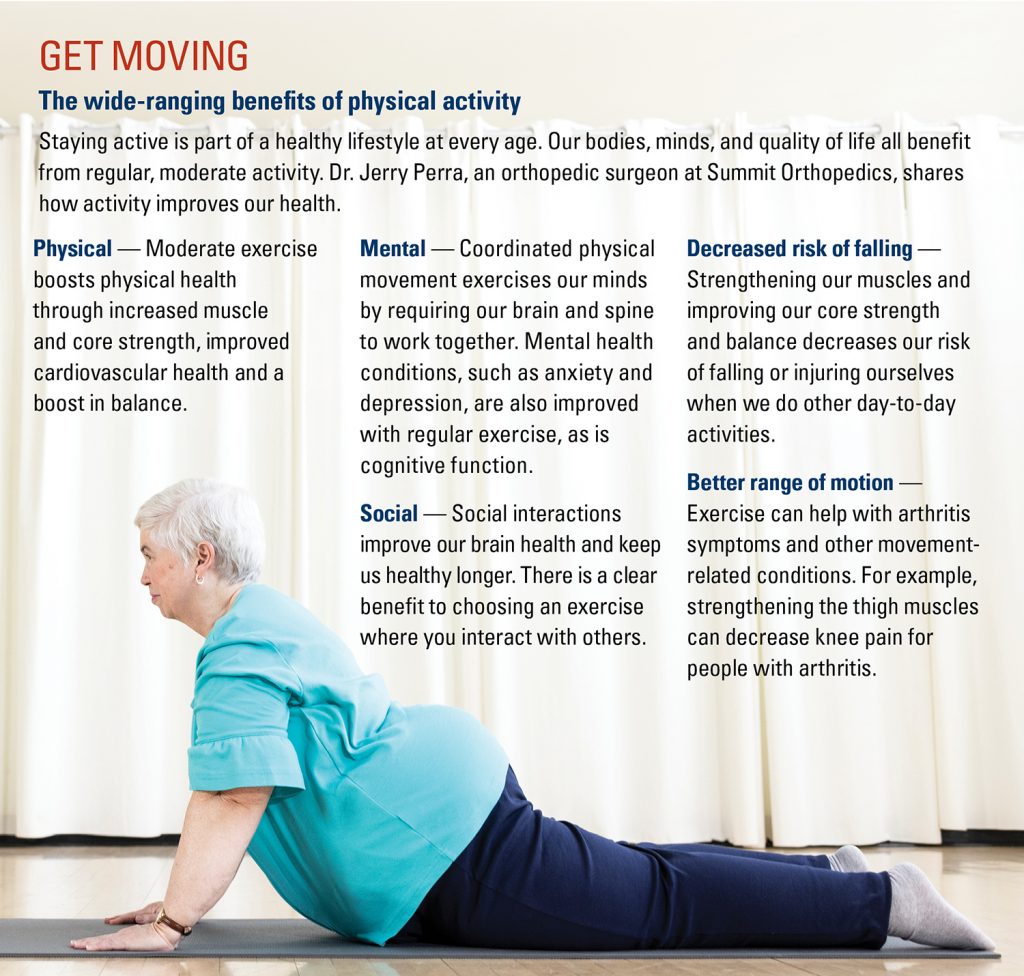
Lingering injuries from those incidents left Little with chronic pain in her back and neck. Arthritis caused joint problems as well, eventually leading to knee replacement surgery. But she hasn’t let pain keep her down. She found relief in exercise, particularly yoga, which she teaches both independently and through Tula Yoga & Wellness in St. Paul.
It has benefited Little in her day-today movements, flexibility, balance and awareness. And most of all, it has helped her prevail over pain.
Little is among more than 100 million people in the U.S. living with chronic pain. Dr. Orlando Charry, a pain medicine specialist for Allina Health, defines the condition as pain that lasts longer than what is expected for a given injury, or pain that goes on for three to six months and impairs quality of life.
While chronic pain is common, it doesn’t need to be accepted. With a multi-pronged approach, Dr. Charry says, pain can be successfully managed and controlled, so it doesn’t rule your life.
Assessing pain
First, Dr. Charry says, it’s important not to let pain go unchecked. Though our bodies are resilient and we can get used to living with aches and pains, that doesn’t mean we should. If you have any chronic pain concerns, be sure to share them with your doctor.
Chronic pain can surface for a wide range of reasons, from injuries to surgery to chronic diseases like diabetes or cancer. It can be skeletal, muscular or organ based. The first step in overcoming it is to acknowledge its presence and assess where it is coming from and why.
Dr. Charry says assessing pain requires a holistic approach. An evaluation covers age, health history, past injuries, lifestyle and more.
The assessment goes well beyond examining the area where the pain is, which would be more inline with addressing acute pain from a recent injury. Pain assessments even include psychological considerations.
“That’s the way we are made,” Dr. Charry says. “Mind, body and spirit in one package. Everything is connected.”
When treating chronic pain, he says, taking that same holistic approach is just as important.
Interdisciplinary treatment
Treating chronic pain usually involves medical professionals from several different specialties. That may include physical therapists, occupational therapists, rehabilitation therapists, health psychologists and others.
“The treatment of chronic pain should be integrated and interdisciplinary,” Charry says. “A comprehensive approach will produce the best outcomes.” Each patient’s situation is unique and will require a different combination of treatment and management efforts. Those might include a combination of medications, physical therapy or other treatments.
For example, doctors might recommend X-rays or nerve studies, could suggest injections such as cortisone shots, might advise a patient to work with a personal trainer who understands the anatomy of a condition, and so on. If a patient is having trouble holding a toothbrush or utensils, or doing other daily activities, an occupational therapist can help find different ways to do those things.
Taking a thoughtful, multi-modal approach to medications is also important, Dr. Charry says.
“Multi-modal means that different types of medications are used for pain, so that they can help each other, in order to try to obtain a better response,” he says.
Common medications for pain treatment include topical creams, acetaminophen (Tylenol), non-steroidal anti-inflammatories, and sometimes steroids, as well as medications for mood. Beyond those are medications that doctors tend to be more cautious about prescribing, Dr. Charry says. Those include adjuvants and muscle relaxants that can cause more serious side effects. Opioids are generally not recommended for chronic pain as they are often abused and can lead to opioid use disorders.
Ongoing physical activity is also a common part of long-term chronic pain management, improving our heart, lung, muscle and bone health. Low impact activities, such as pool exercises or yoga, are great examples of ways to keep our bodies strong and flexible, while also reversing pain symptoms.
“Exercise is a mainstay for any treatment plan, not just to manage pain, but also to prevent it and maintain a healthy lifestyle in general,” Dr. Charry says.
Rising to a challenge
Though Little had tried yoga many years ago, her work life got in the way of making it a habit. It wasn’t until her 60s that she gave it another try — and realized what she’d been missing.
The style she practices and teaches, called SomaYoga, uses slow, gentle movements designed to be therapeutic, releasing tense muscles and promoting healing. She discovered the practice through Tula Yoga & Wellness and quickly recognized the benefits.
“It’s just made life easier. It’s easier to get around. I feel like I’ve slowed the trajectory to old age, so to speak,” Little says. “My mobility is greater, my flexibility is greater, and in general, I have the ability to do things with ease that I wouldn’t be able to do if I hadn’t been doing yoga.”
Her pain isn’t gone, but when symptoms arise, she knows how to move in ways that will help. In addition to practicing yoga about four times a week, Little sees a chiropractor to help with her back pain.
She has also taken up pilates and is learning QiGong. She enjoys the challenge of a new activity as well as the social aspect. She’s met many new friends through her activities and enjoys being a part of the yoga community.
“I enjoy the social contact, the multiple health benefits derived from being active, and the sense of accomplishment when I can finally do something that I wasn’t previously able to do,” she says. “Plus, it just makes me feel good and boosts my mood.”


